Elaine Lai-Han Leung, Cancer Center, Faculty of Health Sciences; MOE Frontiers Science Center for Precision Oncology, University of Macau, Macau (SAR) 999078, China. E-mail: lhleung@um.edu.mo
Abstract
Aims: To assess the influence of age, cancer type, and diverse risk factors on the occurrence of postoperative pulmonary infection (PPI) in patients undergoing thoracic surgery.
Methods: The study encompassed a cohort of 231 patients who underwent thoracic surgery. These patients were randomly divided into two groups: a modeling population comprising 185 patients and a validation population comprising 46 patients, using a random number method at a ratio of 4:1. Bivariate logistic regression models were utilized to discern variables independently predictive of postoperative complications, utilizing SPSS 26.0 (SPSS Institute, Inc., Chicago, IL, USA).
Results: The analysis unveiled that male patients, individuals aged 65 years or older, and those with a history of smoking or chronic obstructive pulmonary disease (COPD) were significantly more predisposed to the development of postoperative pneumonia. Conversely, diabetes and hypertension were not identified as risk factors. Patients with extended intubation times, higher peri-operative bleeding, prolonged hospitalization, and longer operating times displayed an increased likelihood of developing postoperative pneumonia. Intriguingly, preoperative treatments like antibiotic administration and aerosol inhalation did not demonstrate a significant reduction in postoperative pneumonia incidence. Hematological assessments revealed that low preoperative albumin (pre-ALB) levels and other specific markers served as potential indicators of postoperative pneumonia. Binary logistic regression analysis identified pulmonary function, intubation duration, intraoperative bleeding, pre-ALB levels post-operation, and the duration of preoperative hospital stay as significant risk factors. A risk model formula was formulated and validated, successfully demonstrating model construction.
Conclusion: These findings underscore the pivotal importance of taking patient age, cancer type, and various risk factors into account when predicting and managing postoperative pneumonia in thoracic surgery patients.
Keywords
1. Introduction
Thoracic surgery is the primary choice for early stage thoracic malignancies[1-3]. While surgery effectively addresses the removal of tumor tissues, the occurrence of postoperative pneumonia remains a common and potentially life-threatening complication associated with thoracic surgery. This complication carries significant implications for patient recovery, mortality rates, and healthcare costs[4,5]. Studies have shown that the mortality rate among patients diagnosed with postoperative pneumonia is four times higher compared to those without such complications[6]. In the context of a globally aging population and an increasing incidence of thoracic cancers, there is a growing need to better understand the risk factors and develop effective strategies for predicting and managing postoperative pneumonia[7]. Despite advancements in surgical techniques, anesthesia, and perioperative care, postoperative pulmonary complications continue to be a major concern for thoracic surgery patients[8]. Identifying high-risk patients and implementing targeted interventions could potentially reduce the incidence and severity of these complications, ultimately leading to improved patient outcomes[9].
Previous research has pinpointed various risk factors for postoperative pneumonia in thoracic surgery patients, including age, gender, smoking history, chronic obstructive pulmonary disease (COPD), diabetes, hypertension, and preoperative pulmonary function[10]. However, the relative contributions of these factors and their interactions in the development of postoperative pneumonia remain incompletely understood. Moreover, many of these reports are over a decade old, and the number of patients in these studies has been insufficient[11]. Furthermore, the effectiveness of preoperative interventions, such as antibiotic use and aerosol inhalation, in reducing postoperative pneumonia incidence is still a subject of debate. Additionally, the potential role of hematology markers in predicting postoperative pneumonia has not been thoroughly explored. Insufficient investigations specific to chest surgery in Chinese patients have left reliable estimates of pneumonia risk unavailable[12]. This lack of data limits the applicability of these findings in the context of Chinese clinical practice.
The development of a clinical prediction model informed by a population-based experience would contribute to optimal
2. Methods
2.1 Study participants
The study encompassed a total of 231 patients with thoracic surgical tumors who were treated at Taihe Hospital in Hubei, China, between 2017 and 2019. Selection followed international diagnostic criteria for pneumonia and thoracic malignancies. These patients were randomly divided into two groups: a modeling population comprising 185 patients and a validation population comprising 46 patients, using a random number method at a ratio of 4:1. The examination of clinical samples was conducted with the approval and certification of the Ethics Committee of Taihe Hospital. Informed consent was obtained from all patients (Reference Number: 2019KS018).
2.2 Inclusion criteria
The study included patients who were diagnosed with pneumonia according to the China National pneumonia diagnostic criteria. These patients had thoracic cancer, a history of thoracotomy, and had undergone appropriate chest computed tomography (CT) examinations.
2.3 Variables of interest
Various factors were investigated and observed in this study, including demographic data (gender, age, and smoking history), medical history (COPD, diabetes, and hypertension), pulmonary characteristics (pulmonary function and ASA classification), preoperative therapy (antibiotics and aerosol inhalation), intraoperative records (surgical methods, intubation time, operating time, and bleeding volume), postoperative options (central venous catheter (CVC), intraoperative guidance tube (IGT), intraoperative urinary catheter (IUC), hospital stay, and preoperative hospitalization time), bacterial species, and hematology test results.
2.4 Statistical analysis
Statistical analyses were performed using SPSS 26.0 (SPSS Institute, Inc., Chicago, IL, USA) and GraphPad Prism 8.0 (GraphPad Software, La Jolla, CA, United States). Bivariate logistic regression modeling was employed to identify variables that were independently predictive of postoperative complications. The variables entered into the models were selected a priori based on a review of the literature and our univariate analysis, which yielded a P < 0.05. Odds ratios and 95% confidence intervals were calculated. Receiver operating characteristic (ROC) curve analysis was conducted to evaluate the diagnostic performance of the risk factors. P less than 0.05 were considered statistically significant[14,15]. The validation group was subsequently included in the regression equation to verify its predictive efficacy.
3. Results
3.1 Basic characteristics of patients meeting the inclusion criteria
Obtaining reliable risk estimates necessitates a substantial dataset due to the unpredictable nature of postoperative pneumonia in thoracic surgery patients. Over the course of two years, 231 patients who underwent thoracic surgery and met the inclusion criteria were enrolled in this study. These surgical procedures encompassed thoracotomy (46 patients, 24.8%) and thoracoscopy (149 patients, 75.1%). Surgical sites included the lung (n = 93, 50.3%), esophagus (n = 75, 40.5%), mediastinum (n = 14, 7.0%), and other locations (n = 4, 2.2%). In the modeling population, there were a total of 185 patients, with 115 (62.16%) being males and 70 (37.84%) females. Among them, 45 (24.32%) patients were 65 years or older, while 140 (75.68%) were less than 60 years of age. In the validation population, thoracic surgery procedures consisted of thoracotomy in 13 patients (28.26%) and thoracoscopy in 33 patients (71.74%). The operative sites included the lung (n = 21, 45.65%), esophagus (n = 21, 45.65%), mediastinum (n = 3, 6.52%), and other locations (n = 1, 2.17%). The gender distribution was 32 (69.57%) men and 14 (30.43%) women, with 8 (17.39%) patients aged 65 years or older, and 38 (82.61%) aged less than 60 years. No significant differences were observed between the modeling and validation groups in terms of gender
3.2 Age as a risk factor for postoperative pneumonia in thoracic surgery patients
The objective of this study was to evaluate the influence of age, cancer type, and various risk factors on the development of postoperative pneumonia in thoracic surgery patients. To achieve this, a heatmap analysis was applied to visually understand the relationships among these factors (Figure 1). Subsequently, continuous variables such as hemoglobin, albumin (ALB), and total protein (TP) were assessed using Mann-Whitney U analysis to identify group differences. Concurrently, categorical variables such as demographic data and medical history were analyzed using crosstab chi-square analysis.
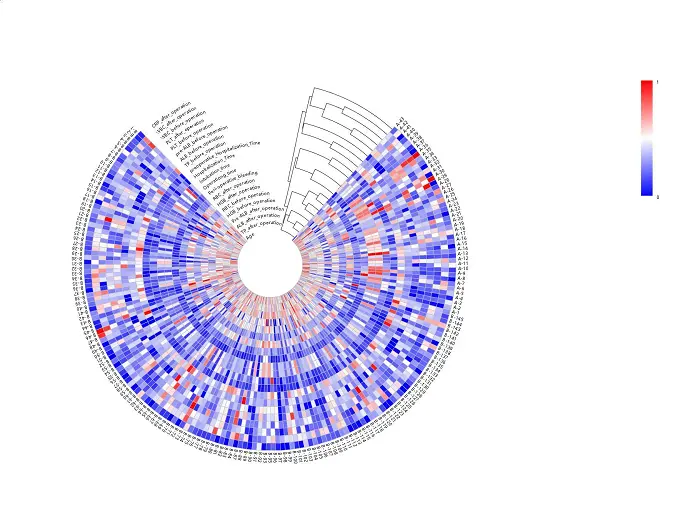
Figure 1. Heatmap depicting the demographic data, intraoperative records and hematology levels of patients with PPI (n = 43) and patients without PPI (n = 142). Patients with thoracic operation were grouped by hierarchical clustering of variables. PPI: postoperative pulmonary infection.
As demonstrated in Table 1, patients aged 65 years or older (37.8%, 17/45) exhibited a higher incidence rate, with a P < 0.001. Moreover, 23.5% (36/115) of male patients had a significantly higher infection rate with a P < 0.001 compared to 10.0% (7/70) of female patients. Analysis of factors related to pulmonary health indicated that patients with a history of smoking and COPD had a significantly higher incidence of infection compared to those without these factors (P < 0.001). In the examination of systemic diseases, neither diabetes nor a history of hypertension was found to be associated with an increased risk of pneumonia (P > 0.05). It was widely acknowledged that patients with reduced pulmonary function and poorer physical condition experienced a significantly higher incidence of infection (P < 0.001)
| Features | Pulmonary infection | All cases | P-value | Features | Pulmonary infection | All cases | P-value | ||
| Yes | No | Yes | No | ||||||
| Gender | 0.001 | Antibiotics | 0.578 | ||||||
| Male | 36 (31.3%) | 79 (68.7%) | 115 (100%) | Yes | 12 (20.7%) | 46 (79.3%) | 58 (100%) | ||
| Female | 7 (10%) | 63 (90%) | 70 (100%) | No | 31 (24.4%) | 96 (75.6%) | 127 (100%) | ||
| Age | 0.008 | Aerosol inhalation | 0.099 | ||||||
| ≥ 65 | 17 (37.8%) | 28 (62.2%) | 45 (100%) | Yes | 38 (25.9%) | 109 (74.1%) | 147 (100%) | ||
| < 65 | 26 (18.6%) | 114 (81.4%) | 140 (100%) | No | 5 (13.2%) | 33 (86.8%) | 38 (100%) | ||
| Smoking history | < 0.001 | Intubation time | < 0.001 | ||||||
| Yes | 34 (37.8%) | 56 (62.2%) | 90 (100%) | ≥ 4.5 h | 31 (39.2%) | 48 (60.8%) | 79 (100%) | ||
| No | 9 (9.5%) | 86 (90.5%) | 95 (100%) | < 4.5 h | 12 (11.3%) | 94 (88.7%) | 106 (100%) | ||
| COPD | < 0.001 | Operating time | < 0.001 | ||||||
| Yes | 17 (73.9%) | 6 (26.1%) | 23 (100%) | ≥ 3.5 h | 35 (33.7%) | 69 (66.3%) | 104 (100%) | ||
| No | 26 (16.0%) | 136 (84.0%) | 162 (100%) | < 3.5 h | 8 (9.9%) | 73 (90.1%) | 81 (100%) | ||
| Diabetes | 0.184 | Peri-operative bleeding | < 0.001 | ||||||
| Yes | 5 (38.5%) | 8 (61.5%) | 13 (100%) | ≥ 200 mL | 33 (40.2%) | 49 (59.8%) | 82 (100%) | ||
| No | 38 (22.1%) | 134 (77.9%) | 172 (100%) | < 200 mL | 10 (9.7%) | 93 (90.3%) | 103 (100%) | ||
| Hypertension | 0.569 | CVC | 0.311 | ||||||
| Yes | 15 (25.9%) | 43 (74.1%) | 58 (100%) | Yes | 30 (25.6%) | 87 (74.4%) | 117 (100%) | ||
| No | 28 (22.0%) | 99 (78.0%) | 127 (100%) | No | 13 (19.1%) | 55 (80.9%) | 68 (100%) | ||
| Pulmonary function | < 0.001 | IGT | < 0.001 | ||||||
| Normal | 13 (9.2%) | 129 (90.8%) | 142 (100%) | Yes | 32 (38.1%) | 52 (61.9%) | 84 (100%) | ||
| Decreased | 30 (69.8%) | 13 (30.2%) | 43 (100%) | No | 11 (10.9%) | 90 (89.1%) | 101 (100%) | ||
| Operation method | 0.011 | IUC | 0.86 | ||||||
| Thoracotomy | 17 (37.0%) | 29 (63.0%) | 46 (100%) | Yes | 34 (22.7%) | 116 (77.3%) | 150 (100%) | ||
| Thoracoscope | 26 (18.7%) | 113 (81.3%) | 139 (100%) | No | 9 (25.7%) | 26 (74.3%) | 35 (100%) | ||
| Hospitalization Time | < 0.001 | ASA classification | 0.001 | ||||||
| 25 days | 27 (45.8%) | 32 (54.2%) | 59 (100%) | Normal | 0 (0.0%) | 2 (100.0%) | 2 (100%) | ||
| ≤ 25 days | 16 (12.7%) | 110 (87.3%) | 126 (100%) | Functional compensation | 31 (19.0%) | 132 (81.0%) | 163 (100%) | ||
| Operative site | 0.005 | Limited physical activity | 12 (60.0%) | 8 (40.0%) | 20 (100%) | ||||
| Lung | 14 (15.1%) | 79 (84.9%) | 93 (100%) | Pre-operative hospital stay | 0.199 | ||||
| Esophagus | 27 (36.0%) | 48 (64.0%) | 75 (100%) | ||||||
| Mediastinum | 2 (15.4%) | 11 (84.6%) | 13 (100%) | ≥ 7 days | 26 (27.1%) | 70 (72.9%) | 96 (100%) | ||
| Other | 0 (0.0%) | 4 (100.0%) | 4 (100%) | < 7 days | 17 (19.1%) | 72 (80.9%) | 89 (100%) | ||
COPD: chronic obstructive pulmonary disease; CVC: central vena catheterization; IGT: indwelling gastric tube. IUC: indwelling urinary catheter.
3.3 Surgery-related factors affecting postoperative pneumonia
Our investigation delved into the factors influencing postoperative pulmonary infections (PPI) during surgery. As delineated in Table 1 and Table S1, patients with longer intubation times, increased perioperative bleeding, extended hospitalization periods, and longer operating times were at a higher risk of developing postoperative pneumonia (P < 0.001). Notably, those who underwent thoracotomy had a higher incidence rate than those who underwent thoracoscopy (P = 0.011). Furthermore, patients with IGT exhibited a significantly higher incidence rate (P < 0.001). However, the presence of IUC and CVC did not significantly affect the incidence of pneumonia (P > 0.05). The location of the operation site was a statistically significant indicator of pulmonary infection (P = 0.005), with esophageal surgery (36.0%) being associated with the highest risk of pulmonary infection in thoracic operations.
3.4 Hematology test indicators for postoperative pneumonia
Postoperative pneumonia exerts a significant impact on patient recovery, mortality rates, and financial costs. Various preoperative therapies, such as antibiotic administration and aerosol inhalation, aim to reduce its incidence. Surprisingly, our study found no significant benefits for patients who received preoperative antibiotics or used aerosol inhalation. Hematology tests are valuable clinical tools, and we investigated their relationship with postoperative pneumonia. As displayed in Table S1, patients with low preoperative ALB levels and low postoperative TP, ALB, pre-ALB, and high C-reactive protein (CRP) levels may indicate a statistically significant risk of pulmonary infection (P < 0.05).
3.5 Identification of potential predictive markers
Variables that displayed statistical significance were employed to construct ROC curves. Based on area under the curve (AUC) values, sensitivity, and specificity, four variables were identified with higher diagnostic value (AUC > 0.700): operating time, perioperative bleeding, intubation time, hospitalization time, pulmonary function, and IGT (Table 2 and Figure S1). These findings suggest that these four continuous variables could serve as potential markers for predicting pulmonary infection.
| AUC | Std. Error | Asymptotic 95% Confidence Interval | Optimal Cut Off | SE (%) | SP (%) | Youden index | ||
| Lower Bound | Upper Bound | |||||||
| ROC analysis of patients with thoracic operation. | ||||||||
| Age | 0.625 | 0.064 | 0.500 | 0.751 | 53.500 | 81.4% | 33.1% | 0.145 |
| Operating Time | 0.739 | 0.054 | 0.610 | 0.821 | 4.340 | 60.5% | 78.2% | 0.387 |
| Intubation Time | 0.747 | 0.055 | 0.641 | 0.854 | 5.330 | 58.1% | 83.8% | 0.419 |
| Peri-operative Bleeding | 0.759 | 0.054 | 0.653 | 0.865 | 190.000 | 76.7% | 65.5% | 0.422 |
| Hospitalization Time | 0.716 | 0.054 | 0.610 | 0.821 | 25.500 | 62.8% | 76.8% | 0.396 |
| Pulmonary Function | 0.795 | 0.056 | 0.685 | 0.904 | 0.500 | 69.8% | 90.8% | 0.606 |
| IGT | 0.703 | 0.056 | 0.001 | 0.593 | 0.500 | 74.4% | 63.4% | 0.378 |
ROC: receiver operating characteristic; AUC: area under the curve; ALB: albumin; IGT: intraoperative guidance tube.
3.6 Binary logistic regression analysis and examination
Variables that exhibited statistical significance in the univariate analysis were incorporated into the binary logistic regression analysis. The results pinpointed pulmonary function, intubation time, intraoperative bleeding, postoperative pre-albumin (ALB), and preoperative hospital stay as risk factors. A risk model formula was developed as follows: P = 3.005 × pulmonary function (0 = normal, 1 = impaired) + 0.828 × intubation time (measured value) + 0.009 × intraoperative bleeding (measured value) - 0.030 × postoperative pre-ALB (measured value) + 0.210 × preoperative hospital stay (measured value) - 3.663. As illustrated in Figure 2, an ROC curve was generated based on the regression outcomes, resulting in an AUC of 0.942 (95% CI: 0.903-0.980), a maximum Youden index of 0.777, a sensitivity of 90.2%, and a specificity of 87.5%. Using this risk model formula, we predicted the risk of postoperative pneumonia for the validation group. The ROC curve derived from the regression results had an AUC of 0.848 (95% CI: 0.685-1.000), a maximum Youden index of 0.625, a sensitivity of 62.5%, and a specificity of 97.3%. These findings confirm the successful construction of the model.
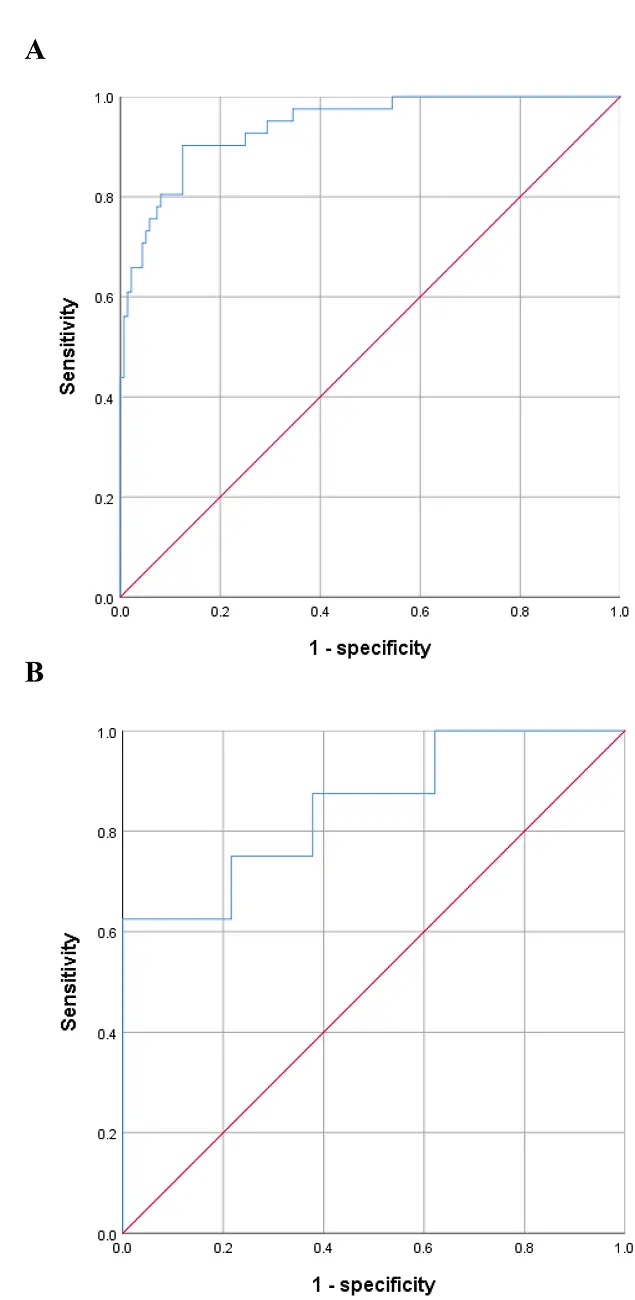
Figure 2. ROC curves for prediction model and model examination. (A) ROC curves for prediction model, the area underneath of ROC curve based on the regression results is 0.942 (95% CI: 0.903-0.980); (B) ROC curves for model examination, the area underneath of ROC curve based on the regression results is 0.848 (95% CI: 0.685-1.000).
3.7 Postoperative pre-ALB: a vital predictor for postoperative pulmonary infection in elderly thoracic cancer patients
Patients aged 65 years or older also exhibited a higher incidence rate, with a P < 0.001. Subsequently, we conducted a more focused analysis on patients aged 65 years and older to create a risk model tailored specifically for this group. The formula for this model is as follows: F = 5.905 - 0.035 × postoperative pre-ALB (measured value). An ROC curve was generated based on the regression results, resulting in an AUC of 0.850 (95% CI: 0.702, 0.999), as illustrated in Figure 3. This model demonstrated a maximum Youden index of 0.732, a sensitivity of 0.875, and a specificity of 0.857. Using the risk model formula, we predicted the risk of postoperative pneumonia for the validation group. The ROC curve, based on the regression results, displayed an AUC of 0.742 (95% CI: 0.565-0.919), as shown in Figure 3. This secondary model exhibited a maximum Youden index of 0.581, a sensitivity of 1, and a specificity of 0.581. These outcomes affirm the successful construction of this specialized risk model.
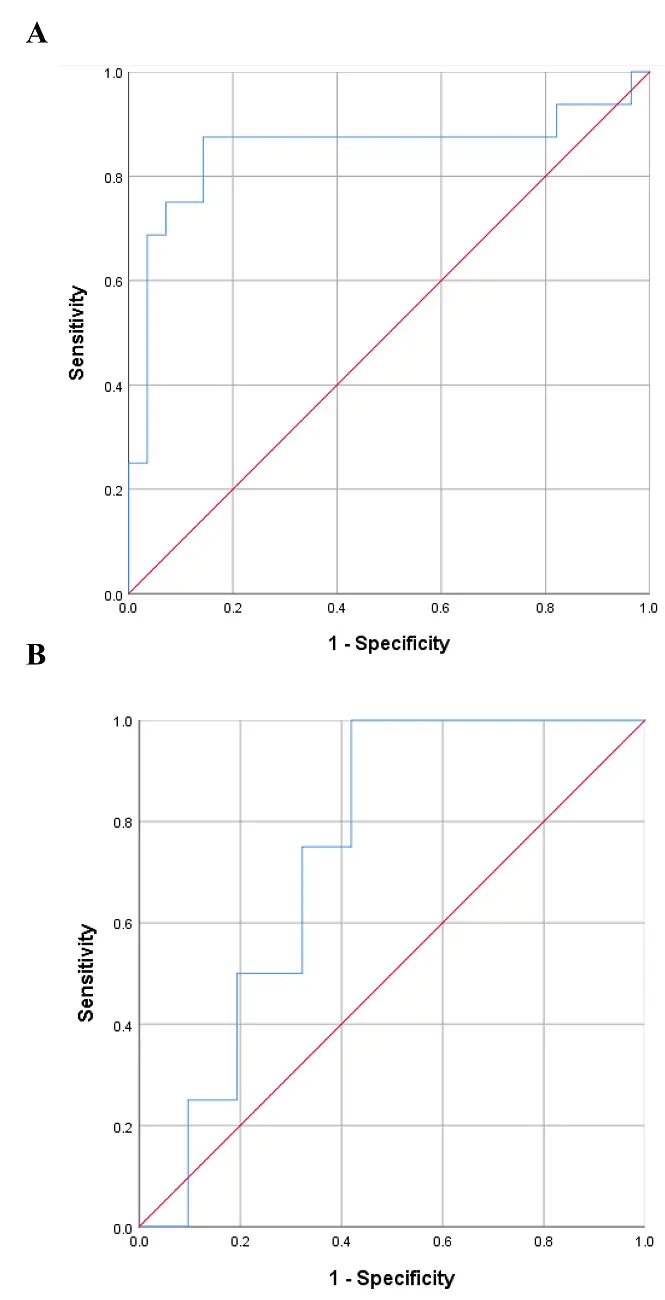
Figure 3. ROC curves for older prediction model and model examination. (A) ROC curves for prediction model, the area underneath of ROC curve based on the regression results is 0.850(95% CI: 0.702, 0.999); (B) ROC curves for model examination, the area underneath of ROC curve based on the regression results is 0.742
3.8 Smoking history and age: two key factors increasing COPD morbidity and impacting systemic function leading to PPI
To comprehensively explore the intricate relationships among age, smoking history, COPD history, and the incidence of PPI, we conducted an analysis as depicted in Figure 4. It became evident that smoking history played a role in triggering COPD, as exemplified by 23 out of 90 (25.56%) patients with a smoking history also having COPD, while none (0%) of the 95 patients without a smoking history exhibited COPD. In an effort to discern the more influential factor between smoking history and COPD, we further investigated the multifaceted connections between them. Among patients with a smoking history, 34 out of 90 (37.78%) experienced pulmonary infection, compared to 9 out of 95 (9.47%) patients without a smoking history. Moreover, among patients with COPD, 17 out of 23 (73.91%) had pulmonary infection, as opposed to 26 out of 162 (16.05%) patients without COPD.
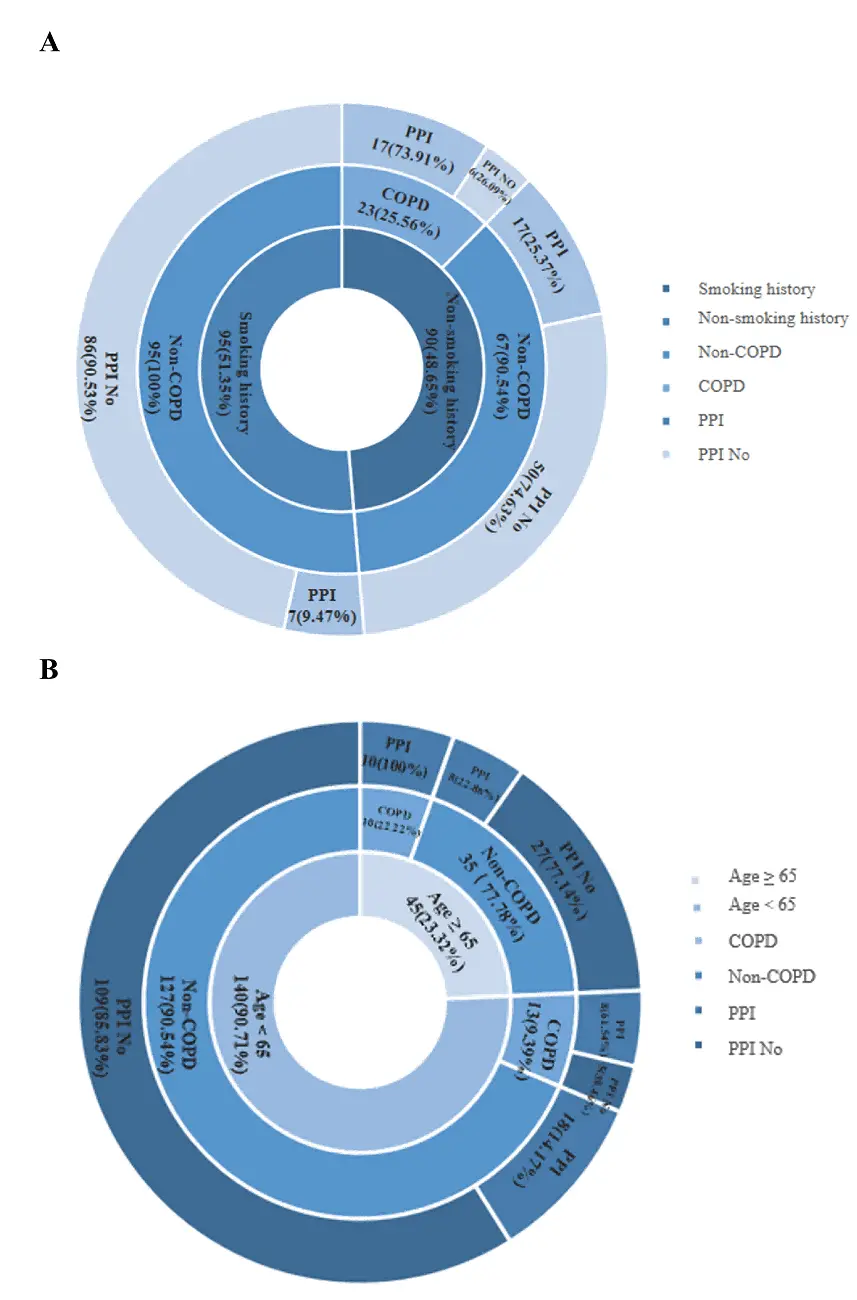
Figure 4. Smoking history and age factor increased morbidity of COPD as well as systemic function of body subsequently inducing PPI. COPD: chronic obstructive pulmonary disease; PPI: postoperative pulmonary infection.
These observations suggest that smoking history contributes to the development of COPD, consistent with existing research findings, and additionally impacts the occurrence of pulmonary infection. Furthermore, this study introduces the hypothesis that age also plays a role in the development of COPD, subsequently influencing the incidence of pulmonary infection. Among patients aged 65 years or older, 10 out of 45 (22.22%) had COPD, while 13 out of 140 (9.29%) patients aged below 65 had COPD. Additionally, 8 out of 35 (22.86%) patients aged 65 or older experienced pulmonary infection, in contrast to 18 out of 127 (14.17%) patients aged below 65.
4. Discussion
Recent reports have highlighted a concerning increase in the incidence of pulmonary infections within hospital settings over the last decade, putting significant strain on public health committees due to the financial burden associated with treating postoperative pulmonary infections[16,17]. This study was conducted with the primary objective of deepening our understanding of the prevalence and characteristics of PPI in both the general thoracic surgery patient population and specifically among elderly individuals with thoracic cancer. Additionally, the findings derived from this study hold the potential to offer valuable insights that can inform the development of effective clinical prevention strategies for mitigating the occurrence of PPI.
Prior research has identified a multitude of risk factors contributing to hospital-acquired infections (HAIs), including conditions such as pneumonia, sepsis/septicemia, and surgical site infections. These risk factors were examined among American patients over the period of 2009 to 2012[18]. That study pinpointed several preoperative factors that heightened the likelihood of HAIs, including being 70 years or older, having a body mass index above 30 kg/m2, cerebrovascular disease, smoking history, hypertension, chronic lung disease, immunosuppressive therapy, peripheral arterial disease, diabetes mellitus, congestive heart failure, and anticoagulant agent use. In a similar vein, our findings revealed several significant risk factors for postoperative pneumonia, including male gender, age ≥ 65 years, smoking history, and COPD. In contrast, conditions such as diabetes and hypertension did not emerge as significant risk factors for postoperative pneumonia. It is noteworthy that patients with impaired pulmonary function and those in poorer physical condition exhibited a markedly higher incidence of postoperative pneumonia. Moreover, individuals with extended intubation periods, higher intraoperative bleeding, prolonged hospitalization times, and longer surgical procedures demonstrated an increased likelihood of developing postoperative pneumonia. Furthermore, we explored the effectiveness of various preoperative therapeutic interventions and examined the potential value of hematology markers as predictive tools for postoperative pneumonia.
Age unequivocally emerges as a substantial risk factor for postoperative pneumonia in patients undergoing thoracic surgery. Our findings are congruent with prior research[19], affirming that patients aged 65 years and older exhibit a significantly higher incidence of postoperative pneumonia when contrasted with their younger counterparts. This escalated susceptibility among older patients can be attributed to a constellation of interconnected factors. Primarily, age-related declines in pulmonary function play a pivotal role, curtailing the body’s ability to effectively ward off postoperative pulmonary complications. Moreover, the efficiency of the immune system diminishes with age, rendering older individuals less capable of defending against infections. The presence of
Smoking during hospitalization is widely acknowledged as a potent risk factor for the development of hospital-acquired pneumonia. The act of smoking promotes the colonization of the airways by pathogenic microorganisms[20,21]. Existing research has demonstrated that patients who abstain from smoking for a minimum of four weeks before undergoing procedures such as coronary artery bypass grafting do not face a higher risk of postoperative pulmonary complications in comparison to individuals who have never smoked[22]. The implications of these findings underscore the value of proactive preoperative counseling on smoking cessation. This approach to counseling extends its protective benefits beyond the immediate postoperative period. Notably, patients who maintain a nonsmoking status for over a week before surgery experience a significantly reduced risk of mortality even up to five years after the procedure[23]. Our study findings accentuate the detrimental effects of smoking in the context of thoracic surgeries, with particular relevance for patients undergoing esophageal operations. Preoperative Antibiotics and Antimicrobial Resistance: In our research, we observed that preoperative interventions, specifically the administration of antibiotics before surgery, had minimal efficacy in preventing PPI. Presently, preoperative interventions aim to target nosocomial pathogens, particularly Gram-negative bacteria. This necessitates the use of broad-spectrum antibiotics like piperacillin-tazobactam. However, this approach carries a dual risk: the potential promotion of antimicrobial resistance in patients and the financial burden associated with the utilization of such potent, broad-spectrum agents. Consequently, our study underscores the paramount importance of accurate diagnosis when dealing with PPI. Ensuring the judicious and appropriate use of antimicrobials becomes imperative. Rather than resorting to preemptive administration of antibiotics, a more prudent approach is warranted, emphasizing precise diagnosis to ensure that antibiotics are only deployed when clearly indicated. This approach not only mitigates the risks associated with antimicrobial resistance but also serves to curtail unnecessary healthcare costs[24]. Consequently, our study underscores the paramount importance of accurate diagnosis when dealing with PPI. Ensuring the judicious and appropriate use of antimicrobials becomes imperative. Rather than resorting to preemptive administration of antibiotics, a more prudent approach is warranted, emphasizing precise diagnosis to ensure that antibiotics are only deployed when clearly indicated.
Our research brings to light that certain preoperative hematology markers-including ALB, pre-ALB, and CRP-serve as significant predictors of postoperative pneumonia in the context of thoracic surgery. Recent studies in various surgical patient groups have unveiled a strong link between preoperative albumin levels and an elevated likelihood of postoperative infectious complications[25]. Our hypothesis posits that patients presenting with low ALB and pre-ALB levels before surgery might be grappling with issues such as malnutrition, COPD, or reduced pulmonary function. In circumstances where the underlying causes of these abnormal ALB and
The predictive factors within our risk model are of particular significance. This model implies that patients with stronger lung function, shorter intubation times, minimal intraoperative bleeding, elevated postoperative pre-ALB levels, and shorter preoperative hospitalization periods exhibit a reduced incidence of postoperative pneumonia. This observation aligns with prior research, including a meta-analysis[26] which underscores the beneficial impact of preoperative breathing exercises on enhancing respiratory function in lung cancer patients. Such exercises have been shown to reduce the incidence of pulmonary complications. In light of these findings, it becomes pertinent to instruct lung cancer patients in preoperative lung function exercises as part of their preparatory regimen. Prolonged intubation times pose an increased risk due to extended exposure to external sources, thereby elevating the likelihood of infection. The relationship between intraoperative bleeding volume and the occurrence of postoperative pneumonia emphasizes the need for strategies to minimize intraoperative bleeding, subsequently reducing the risk of pneumonia. Additionally, the influence of preoperative hospitalization duration on PPI incidence might be attributed to an elevated risk of nosocomial-acquired pneumonia with extended stays. Alternatively, it could be correlated with the fact that prolonged bed rest during hospitalization for lung cancer patients results in poor sputum clearance, potentially contributing to heightened lung infection risks in the postoperative period. Understanding and acknowledging these predictive factors, clinicians can adopt strategic measures to enhance patient safety and reduce the occurrence of postoperative pneumonia in thoracic surgery patients.
It’s important to recognize that our current study has several limitations. It’s primarily a single-center retrospective study, which naturally restricts the generalizability of the findings and the ability to establish causality. This limitation is inherent in the study’s design and impacts the broader applicability of our results. Moreover, the reasons behind the increased morbidity of PPI following aerosol inhalation pretreatment remain unclear. This specific area presents a knowledge gap, and we were unable to elucidate whether the aerosol inhalation machine might be contributing to this elevated risk factor within the scope of our study[27]. Another limitation arises from the challenge of establishing a causal relationship between the duration of hospital stay and the incidence of PPI. Although prolonged hospitalization is a known risk factor for nosocomial-acquired pneumonia, the precise reasons for the increased morbidity of PPI after aerosol inhalation pretreatment are yet to be fully understood. Despite these limitations, it’s essential to underscore that this investigation can still provide valuable insights and inform clinician-patient decision-making. It serves as an important resource for healthcare professionals seeking to mitigate the risk of PPI. Our study identifies specific predictive factors, including hematology levels, intraoperative records, and demographic data, which can be effectively utilized in a clinical setting. These variables are demonstrably valuable for patient risk assessment and can guide clinical decision-making. Consequently, our findings offer a practical framework for enhancing patient safety and reducing the incidence of postoperative pneumonia in thoracic surgery patients, despite the study’s inherent limitations.
In conclusion, patients who are younger without smoking history and with stronger lung function, shorter intubation times, minimal intraoperative bleeding, elevated postoperative pre-ALB levels, and shorter preoperative hospitalization periods exhibit a reduced incidence of postoperative pneumonia.
Supplementary materials
The supplementary material for this article is available at: Supplementary materials.
Authors contribution
Tang YJ, Leung ELH: Conceptualization.
Tang YJ, Liu L: Project management.
Hu WW, Cai LL, Wang MF, Zhang J, Guo JL: Resources.
Li RZ, Lian LR, Hu WW, Cai LL: Data curation.
Li RZ, Lian LR: Formal analysis.
All authors participated in manuscript writing and final approval of manuscript.
Conflicts of interest
The authors declare no conflicts of interest.
Ethical approval
The examination of clinical samples was conducted with the approval and certification of the Ethics Committee of Taihe Hospital. Informed consent was obtained from all patients (Reference Number: 2019KS018).
Consent to participate
Informed consent was obtained from all patients.
Consent for publication
Not applicable.
Availability of data and materials
The data and materials could be obtained from the corresponding author.
Funding
This study was supported by the Macau Science and Technology Development Fund (FDCT-0096/2018/A3, 0063-2022-A2) and the National Natural Science Foundation of China (81828013, 82204677, 82230119). Additional support was provided by the Science and Technology Projects in Guangzhou (SL2022A04J00459), the Technology Research Projects of the State Key Laboratory of Dampness Syndrome of Chinese Medicine (SZ2022KF20), and the Traditional Chinese Medicine Bureau of Guangdong Province Project (20241112). This study also received funding from the 2020 Young Qihuang Scholar program of the National Administration of Traditional Chinese Medicine, a start-up research grant (SRG2022-00020-FHS), and the Faculty of Health Sciences, University of Macau.
Copyright
© The Author(s) 2023.
References
-
1. Mönig S, Chevallay M, Niclauss N, Zilli T, Fang W, Bansal A, et al. Early esophageal cancer: the significance of surgery, endoscopy, and chemoradiation. Ann N Y Acad Sci. 2018;1434(1):115-123.[DOI]
-
2. Pennathur A, Brunelli A, Criner GJ, Keshavarz H, Mazzone P, Walsh G, et al. Definition and assessment of high risk in patients considered for lobectomy for stage I non-small cell lung cancer: the American Association for Thoracic Surgery expert panel consensus document. J Thorac Cardiovasc Surg. 2021;162(6):1605-1618.[DOI]
-
3. Roden AC, Ahmad U, Cardillo G, Girard N, Jain D, Marom EM, et al. Thymic carcinomas-a concise multidisciplinary update on recent developments from the thymic carcinoma working group of the international thymic malignancy interest group. J Thorac Oncol. 2022;17(5):637-650.[DOI]
-
4. Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118(3):317-334.[DOI]
-
5. Arozullah AM, Khuri SF, Henderson WG, Daley J. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med. 2001;135(10):847-857.[DOI]
-
6. Hortal J, Giannella M, Pérez MJ, Barrio JM, Desco M, Bouza E, et al. Incidence and risk factors for ventilator-associated pneumonia after major heart surgery. Intensive Care Med. 2009;35(9):1518-1525.[DOI]
-
7. Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144(8):581-595.[DOI]
-
8. Agostini P, Cieslik H, Rathinam S, Bishay E, Kalkat MS, Rajesh PB, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax. 2010;65(9):815-818.[DOI]
-
9. Canet J, Mazo V. Postoperative pulmonary complications. Minerva anestesiol. 2010;76(2):138-143.[PubMed]
-
10. Allou N, Bronchard R, Guglielminotti J, Dilly MP, Provenchere S, Lucet JC, et al. Risk factors for postoperative pneumonia after cardiac surgery and development of a preoperative risk score. Crit Care Med. 2014;42(5):1150-1156.[DOI]
-
11. Santos M, Braga JU, Gomes RV, Werneck GL. Predictive factors for pneumonia onset after cardiac surgery in Rio de Janeiro, Brazil. Infect Control Hosp Epidemiol. 2007;28(4):382-388.[DOI]
-
12. Kinlin LM, Kirchner C, Zhang H, Daley J, Fisman DN. Derivation and validation of a clinical prediction rule for nosocomial pneumonia after coronary artery bypass graft surgery. Clin Infect Dis. 2010;50(4):493-501.[DOI]
-
13. Strobel RJ, Liang QX, Zhang M, Wu XT, Rogers MAM, Theurer PF, et al. A preoperative risk model for postoperative pneumonia after coronary artery bypass grafting. Ann Thorac Surg. 2016;102(4):1213-1219.[DOI]
-
14. Wang M, Wang S, Song Z, Ji X, Zhang Z, Zhou J, et al. Associations of IL-4, IL-4R, and IL-13 gene polymorphisms in coal workers’ pneumoconiosis in China: a case-control study. PLoS One. 2011;6(8):e22624.[DOI]
-
15. Kuo HW, Chang CL, Lai JS, Lee FC, Chung BC, Chen CJ. Prevalence of and factors related to pneumoconiosis among foundry workers in central Taiwan. Sci Total Environ. 1998;222(3):133-139.[DOI]
-
16. Chen KY, Ko SC, Hsueh PR, Luh KT, Yang PC. Pulmonary fungal infection: emphasis on microbiological spectra, patient outcome, and prognostic factors. Chest. 2001;120(1):177-184.[DOI]
-
17. LaPar DJ, Crosby IK, Rich JB, Fonner E, Kron IL, Ailawadi G, et al. A contemporary cost analysis of postoperative morbidity after coronary artery bypass grafting with and without concomitant aortic valve replacement to improve patient quality and cost-effective care. Ann Thorac Surg. 2013;96(5):1621-1627.[DOI]
-
18. Shih T, Zhang M, Kommareddi M, Boeve TJ, Harrington SD, Holmes RJ, et al. Center-level variation in infection rates after coronary artery bypass grafting. Circ Cardiovasc Qual Outcomes. 2014;7(4):567-573.[DOI]
-
19. Vasudevan K, Grossberg JA, Spader HS, Torabi R, Oyelese AA. Age increases the risk of immediate postoperative dysphagia and pneumonia after odontoid screw fixation. Clin Neurol Neurosurg. 2014;126:185-189.[DOI]
-
20. Garibaldi RA, Britt MR, Coleman ML, Reading JC, Pace NL. Risk factors for postoperative pneumonia. Am J Med. 1981;70(3):677-680.[DOI]
-
21. Rotstein C, Evans G, Born A, Grossman R, Light RB, Magderet S, et al. Clinical practice guidelines for hospital-acquired pneumonia and ventilator-associated pneumonia in adults. Can J Infect Dis Med Microbiol. 2008;19(1):19-53.[DOI]
-
22. Al-Sarraf N, Thalib L, Hughes A, Tolan M, Young V, McGovern E. Effect of smoking on short-term outcome of patients undergoing coronary artery bypass surgery. Ann Thorac Surg. 2008;86(2):517-523.[DOI]
-
23. Vlietstra RE, Kronmal RA, Oberman A, Frye RL, Killip T. Effect of cigarette smoking on survival of patients with angiographically documented coronary artery disease. Report from the CASS registry. JAMA. 1986;255(8):1023-1027.[PubMed]
-
24. Russell CD, Koch O, Laurenson IF, O’Shea DT, Sutherland R, Mackintosh CL. Diagnosis and features of hospital-acquired pneumonia: a retrospective cohort study. J Hosp Infect. 2016;92(3):273-279.[DOI]
-
25. Benton MJ, Wagner CL, Alexander JL. Relationship between body mass index, nutrition, strength, and function in elderly individuals with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2010;30(4):260-263.[DOI]
-
26. Wang YQ, Liu X, Jia Y, Xie J. Impact of breathing exercises in subjects with lung cancer undergoing surgical resection: A systematic review and meta-analysis. J Clin Nurs. 2019;28(5-6):717-732.[DOI]
-
27. Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370(13):1198-1208.[DOI]
Copyright
© The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Publisher’s Note
Share And Cite



