Abstract
The demand for advanced cosmetics needed for remodeling to enhance beauty and fashion is on the increase in modern times. Also, some of the major parts of the human head that bring about great discomfort in the human body if not put in proper conditions are the teeth, nose, ears, and eyes. Among these parts, the teeth are highly susceptible to serious attack and damage at various stages of life. To date, pleasurable feeding would be practically impossible for humans without the aid of teeth that are responsible for cutting and chewing. However, as with other parts of the human body, there are always issues affecting the maxillofacial prosthesis and teeth, which are usually the result of aging, accidents, or diseases. These issues influence the rising need for the replacement of maxillofacial and dental bones with different materials that are developed to meet the structural and biocompatibility needs. Facial and dental implantations have brought about many modifications to human appearance in recent times. The implants are expected to be safe and acceptable to the body system as the patient grows since growth is crucial to human existence. As, growth is a function of the age group in human beings and, the three major age groups respond to growth at different rates. Thus, this review considers the influence of the human age group on maxillofacial and dental implants. The review provides an insight to the demand from each age group and the necessary guides on the selection of appropriate biomaterials as well as future expectations for maxillofacial and dental bones. This is essential because adequate knowledge of the age group of the patients who need maxillofacial and dental bones demands accurate prescriptions.
Keywords
1. Introduction
The human being has 32 teeth in adulthood as well as multiple facial bones of different sizes in the skull[1]. These teeth are part of the skeletal system and are primarily responsible for mastication, chewing, and grinding of food, which humans require to survive.
Due to continuous usage and ageing, maxillofacial bones and teeth are repeatedly subjected to infections and accidents, which sometimes lead to gradual degradation and ultimately wear-off or fracture if not properly maintained. Chemical and organic materials also affect the teeth and maxillofacial bones in a variety of ways and, if not curbed, could bring about bacterial and viral infections and other related diseases that may eventually result in the displacement or loss of the maxillofacial bones or the teeth. These infections can be prevented or avoided in the teeth by proper cleaning and maintenance, whereas in the maxillofacial bones, individuals must focus on accident prevention and less use of inorganic chemicals[2].
The facial bones and human teeth are also prone to accidents during daily activities; accidents can result in a fracture or outright removal of the affected maxillofacial bone. Any of these factors could result in different levels of discomfort since the affected bone or tooth (as the case may be) is no longer capable of performing its function as required. The use of osseointegrated, dental, and maxillofacial implants helps reduce the adverse effects of damaged facial bones and teeth[3,4]. The main applications for osseointegrated implants are present in dentistry to offer a strong base for prosthetic devices and are also frequently used to replace lost teeth. The capacity of osseointegrated implants to fuse with the surrounding bone tissue (gum) is a crucial characteristic expected of any implantation materials. Hence, the selection of appropriate materials is very essential. Once the implant is surgically inserted into the gum, osseointegration takes place over time to forge a solid and long-lasting bond between the implant and the bone[3,4]. Biocompatible materials, such as titanium and titanium oxides are commonly used in osseointegrated implants to facilitate osseointegration and reduce the likelihood of rejection. For cosmetic or reconstructive applications, facial implants are made to improve or repair facial features. Because these implants give volume and contour to particular facial locations, they are frequently utilized to treat congenital abnormalities, injuries, or aesthetic problems. However, facial implants do not fuse with the bone, in contrast to osseointegrated implants. Rather, they provide a more surface-level enhancement to the facial structure by being positioned beneath the skin and soft tissues. Common facial implants are used to improve or repair particular facial characteristics including cheek, chin, and jaw implants[3,4].
Nevertheless, the implant needs of each individual vary due to several factors, ranging from the age of the individual, the size of the individual's jaw, and other physical facial features as well as the nature of the individual's maxillofacial defects or infection[3,4]. These factors influence the type of implant needed by each individual, as well as the type of usage and maintenance required. Various maxillofacial implants exist for different human age ranges to fix the vast variety of maxillofacial defects that occur in the human face[4,5]. These implants are manufactured with different materials, which must be biocompatible and bioactive to reduce the deleterious effects that may result from introducing foreign materials into the human body.
There are several notable differences in the dental and facial bone replacement requirements for adolescents and adults. For instance, temporary/milk teeth and permanent teeth are for different age groups. Within the age of children/adolescence, any temporary/milk teeth that are removed can be replaced naturally while at the adult stage, the permanent teeth cannot be replaced naturally after removal. These are primarily due to the ability of teeth bones to regrow until the human being crosses a certain age limit, after which the tooth no longer has the growth potential once removed[6]. These differences must be taken into account when recommending implants or prosthetics for use in dental and other maxillofacial reconstruction applications. As a result, appropriate technology must be used to develop suitable materials[7]. Composite material development has been identified as a viable process for influencing our environments to meet human desires[8]. The types of materials used in developing implants play a major role in the rate of healing as well as tissue integration[9]. However, the age of the individual determines, to a large extent, how the body heals over the implants[10,4]. Though more of the implantations are carried out on the adults. Occasionally, some younger ones with diseased or accidental cases have usually been handled as well, hence, the inclusion of every group in this review.
Polymeric composites (including silicon-based polymers) are now playing an important role in the development of biomaterials for the biomedical industry, thanks to advanced research on polymer-based composites. Advanced materials are presently being developed to replace costly and scarce materials and also serve as a replacement for other materials in areas of applications where polymers were formerly considered unsuitable. Polymeric-based products have recently replaced metals and ceramics in construction, aviation, automobiles, and biomedical applications[11]. The biocompatibility of polymers and the apparent ease and convenience of forming polymer-based composites have propelled their use in several biomedical applications, including the development and construction of dental and maxillofacial implants. Thus, this class of materials is fast becoming the most suitable for meeting human needs for dental, maxillofacial, and subdermal applications.
To meet human yearning in recent times, where high demand has been placed on the modification of body parts, in particular, the human face to enhance beauty and aesthetics, maxillofacial prosthesis and dental implantations have played many roles. It has contributed a lot to the fashion and health care delivery services and needs in the modern age and hopefully, as more demands on cosmetics globally increase, facial and dental implantations will continue to require more attention from researchers. Hence, this review was to aid further research and development in this field with a strong emphasis on the influence of age and growth on the implants.
2. Dental Implants and Age Ranges
2.1 Childhood
Implant dentistry has recently shown interest in the artificial and permanent replacement of lost teeth in adolescents and adults. This implant's benefits and long-term acceptance are the reasons for its widespread use[10]. In the previous two decades, the prosthetic replacement of human teeth by dental implant materials was primarily limited to patients (primarily adults) with complete craniofacial growth; thus, an individual below the adulthood range would not be administered a dental implant replacement[12]. Successful implantation in older patients with dental ailments naturally depends on the treatment plan, the quality and quantity of the bone, good long-term oral hygiene, sound surgical technique, and optical restorative prostheses. These "success dependents" also apply to children, but children uniquely have steady growth in bone and bone mineral density[13]. The replacement of a damaged adult tooth by the insertion of dental implant material cannot be overemphasized in the treatment of dental ailments in the world today. In children, this thermal treatment method has not been considered seriously, and the use of implants is still infrequent and controversial[14]. In some cases, anodontia, partial anodontia, congenitally missing teeth, and tooth loss from accident or trauma occur in children and adolescents, and they may undergo dental implantation with a dental implant that would be thoroughly scrutinized to suit the body system and growth rate of the patient. However, part of the reason for low dental implantation demand at this age group can based on the fact that the teeth at this stage are usually temporary, and if removed, the possibility of it been replace naturally with permanent teeth is certain. Also, based on human activities, children are less susceptible to human-induced hazards compared to adolescents and adults[15]. The use of implants in this stage is only in rare cases, especially if the patient has an underlying disease like Leukemia or cancer, which is still a whole controversy in the medical field.
The use of implant dentistry in paediatric patients varies greatly as individuals progress through the stages of development. Existing literature revealed growth in children's dentition that can bring about changes even at the jaw bones with the exclusion of muscles around dental implantation[16]. This process is expected to result in infra-occlusion of the implant-assisted prosthesis relative to the rest of the dentition. This stage has been identified as the primary threat, and it is the reason why the growth of implant dentistry in paediatric dentistry has been initially limited. Despite this, some studies have shown implant material insertion and effective control of infra-occlusion in growing children[10].
Major indicators of the need for dental implant placement in growing patients can be divided into two categories:
i. Congenital (which includes non-syndromic hypodontia, ectodermal dysplasia, and cleft lip and palate)[10,14].
ii. Acquired (which includes lost teeth through dentoalveolar trauma and tumour resection)[15].
The presence of adjacent primary teeth, skeletal growth of the jaw bone, insufficient quantity, low-quality mandibular bones, poor dental hygiene, and a poor mental state are all inherent alterations to dental implant insertion in paediatric patients[13].
One of the most important factors that should be considered during dental implantation in children is skeletal maturation. To minimize infra-occlusion, which is assessed using hand-wrist radiographs or a cephalometric analyzer, this requires careful consideration. Methods for managing infra-occluded implants were worked on by Kamatham et al.[10], in which they concluded that the essential methods involve novel implant-borne prosthetic restoration, orthodontic pre-treatment to alter adjacent teeth, as well as extrusion of divergent teeth and distraction osteogenesis.
An innovative implantation-borne prosthetic restoration has been successfully used in the management of infra-occlusion, and the crown-root ratio has been identified as a factor that may influence the prognosis of this new implant-borne prosthetic restoration[17]. However, there are certain limitations with this new technique in the management of infra-occlusion in children, which include.
i. Infection.
ii. Undesirable shape.
iii. Delayed consolidation that led to non-union.
iv. Premature consolidation and incomplete osteotomy.
v. Unwanted lingual/palatal inclination of the transported bony segment relative to basal bone[18].
As a result, more clinical studies should be conducted to regulate the predictability of using this management in children. Dentists are not to contraindicate the application of dental implantations in children to avoid infra-occlusion since previous investigations of craniofacial dimensions have established major changes during their adulthood stage[19]. Therefore, the benefits of dental implantations should always be weighed against their simultaneous difficulties. Whenever dental implants are inserted into the jaw of a child, enhanced aesthetics, reduced bone loss, function, and dental hygiene are the main benefits, in addition to the psychological comfort of the child[20]. Restoration with implants advances the self-esteem of children or adolescents, which is an important factor supporting the application of implants[10]. If children are in their active growth phase, a special type of biocompatible implant material known as mini implants has been proven to be an alternative treatment procedure carried out to achieve an aesthetic and functional achievement. This treatment procedure is suitable because they can be detached or unscrewed with ease when they are infra-occluded. Thus, this aids the preservation method of handling ailments in paediatric dentistry and thereby, providing successful dental implantation in the growth phase[21].
Kumari et al.[22], in their study on dental implants in children concluded that during the implantation procedure of a damaged tooth that is adjacent to another set of teeth, a dentoalveolar growth arises in the edentulous space. When a dental implant is placed prior to dentoalveolar growth, it becomes immersed relative to adjacent teeth, confirming that dental implant materials have the same physiological properties as an ankylosed tooth, resulting in poor aesthetics and implant-to-crown ratio. To mitigate these issues in children and adolescents, it is essentially suggested that dental implants in children should not be administered until two-year cephalograms indicate an absence of alteration in the position of the adjacent teeth[23]. Any missing tooth or set of teeth with adjacent permanent teeth in growing pediatric patients can be treated with dental implantation using a specially selected material[24]. Future dentoalveolar growth as well as the patient's psychological maturity must be carefully considered during the preparation for dental implant placement (commonly known as pre-implantation activities) in children. On occasion, an edentulous arch occurs, and since there are no teeth present, less attention is shown to the dentoalveolar growth. The major focus in this situation is the vertical development of the complete mandible, which most times leads to incoherence in jaw size due to mandibular rotation, though the location of implant material usually shows less effect[12].
In as much as necessary and cautious considerations are given to the physical and psychological growth of paediatric patients before dental implantation is carried out, it is very necessary and of good ethics for paediatric patients to recognize and appreciate oral hygiene techniques and also execute them effectively. In growing patients, oral hygiene has undoubtedly become less effective, and dental implantation is rarely carried out[19].
Laboratory studies made on the physiological characteristics of jaw growth have indicated that it is advisable to exclude implant placement sequel to the mandibular canines[25]. Dental implants have also been implanted effectively in growing patients with ectodermal dysplasia. It is critical to note that the use of implant materials in growing children requires extreme caution because the development of the jaws and dentition occurs frequently. On rare occasions and when other options are available, dental implantation should be avoided until the adolescent age of 15 for females and 18 for males[22]. Patients who have undergone any form of dental implantation should also undergo sufficient follow-ups to locate or prevent any possibility of infection. Though fewer accidents and cases of self-abuse are expected to cause problems at this stage, diseases have always been a major challenge. The use of implants for children is usually only done in exceptional or specific cases and is not very common in clinical practice. Due to the growth at this age, biomedical implants that can regenerate and grow with the patient are desirable to eliminate the need for follow-up. Such advanced materials are needed for this purpose and age[25].
2.2 Adolescence
In a 10-year follow-up investigation that was excluded from the review because the reason for implant placement was not specified, 47 implants were inserted in patients between 13 and 17 years of age. The output showed dental implantation as an effective procedure for treating or replacing missing teeth in adolescence[26]. In their study on the Orthodontic characteristics of the application of oral implants in adolescents, Thilander et al.[26], mentioned a few important points. The maxillary incisor region, especially the lateral incisors in adolescence, is more susceptible to adverse effects caused by the constant development of adjacent teeth and craniofacial growth after the adolescent stage. Hence, the adolescent stage is known as the critical age for implant placement[27]. Also, another factor that influences an adverse effect on dental implants in adolescents is the presence of space between the implant material and adjacent teeth[28]. It was discovered that a smaller distance between a dental implant and an adjacent tooth in adolescents brings about a greater risk of bone loss around implant material[10]. Therefore, the acquisition of adequate space for dental implant placement prior to extraction is a vital step that brings about a positive impact during post-implantation stages in adolescents[29]. The large distance between the implants reduced the success rate of the implantation. Hence, before placing implants in adolescents, appropriate space must be available in the implant site by uprighting and paralleling adjacent teeth with the aid of non-intrusive movements[30].
Ledermann et al.[31], reviewed 42 implantations in 34 patients with an average age of 15 years, and it was concluded that a 90% success rate at a follow-up time of about 36 months was obtained in their study. The investigation revealed a positive soft and osseous tissue reaction to osseointegrated dental implants. A major difficulty was discovered, which was stated to be the ankylotic nature of dental osseointegrated implant material and its inability to react to the vertical growth of adjacent teeth and the alveolus, which resulted in infra-occlusion of implantation.
It is important to consider certain factors when introducing dental implant materials to growing patients (children and adolescents). Therefore, great attention must be paid when placing dental implant materials in growing patients due to physical and developmental alterations of the jaws, chin, and entire dentition. The introduction of implant materials should be delayed if possible until 15 and 18 years of age for females and males, respectively. Finally, growing patients who have been previously treated with dental implants should be given a suitable follow-up[13].
2.3 Adulthood
As concluded by various researchers, achievement in biological implant therapy is mainly grounded on the durability and physical stability of tissue integration with bone. One of the major physical and biological concerns in administering dental implants to adult patients is the possibility of compromised healing of the surgery-related wound that accompanies implantation as well as the effect of ageing on the long-term integrity of osseointegration[32]. Implant-supported crowns of an adult can cause submergence, inconsistencies of marginal gingivae, an upwardly curved distortion of the intercuspid occlusal plane, a compensatory eruption of mandibular incisors, and mesial tipping of maxillary lateral incisors and canines. These complications due to compromised healing can cause great discomfort to patients.
Osseointegration in implant dentistry is a complicated process that involves a group of intertwined procedures that take place when the root of the implant is in contact with the tissue[32]. This tissue-implant relationship involves the blood-clot formation and primary adsorption of serum constituents prior to implantation and immune-inflammatory response to implant insertion. Mobility and connection of undifferentiated mesenchymal cells onto the implant surface, their proliferation and differentiation formation of extracellular matrix, and finally, their mineralization and maturation. Research carried out with the use of a human in vivo model also confirmed skeletogenesis, inflammation, neurogenesis, and angiogenesis as the main biological procedures involved in osseointegration[33].
The physiologic and biological process of ageing from early adulthood to late adulthood is also very complicated at molecular stages. The cellular and systemic stages also influence the characteristics and procedures of healing the affected areas associated with dental implantation. Ageing in adult patients has been confirmed to have a vital impact on the healing process of other soft and hard tissues affected by dental implantation. This ageing factor is also associated with the deterioration of other parts of the human body, such as skin wrinkles and long bone fractures[34]. Inflammation in the human body is a vital aspect to be considered, which is also the genesis of injury healing, and this has been proven to rise with age in adults[35]. In adults, ageing has been reported to catalyze the release of inflammatory hormones from fibroblasts. Thus, a protracted inflammatory period in the human body might as well delay wound healing following dental implantation[32].
The healing of soft tissues after dental implants are administered to adults begins after 2 weeks of insertion; thereafter, fibroblasts, which are known as the predominant cells found in the connective tissue interface, begin to heal and take about 4 weeks to stabilize. As the connective tissue starts to develop, the density of fibroblasts undergoes a steady decrease. Depending on the adulthood stage, after 6 to 8 weeks of healing, a developed barrier of the epithelium as well as copiously structured collagen fibres become evident; thus, a complete and efficient soft-tissue seal is developed[36]. However, dental reconstruction of an ablative defect in a young adult male that was initiated by the resection of an ameloblastoma in the mandible has been reported[37]. Though, Hawley material and a buccal resin-bonded retainer were used in this case, an overeruption of maxillary posterior teeth occurred, which almost led to the obliteration of the intermaxillary gap. Thus, during the healing process of dental implantation, proper care should be taken to avoid complications.
Two phases of ageing can influence new tissue formation during the regenerative phase of healing, which includes alterations in stem cell populations and the microenvironment (growth factors, extracellular matrix, etc.), and these changes influence the biological activity of progenitor cells[38-42]. The population of stem cells within the micro-environment is directly influenced by the surface roughness of the base implant, which provides a suitable environment or scaffold for cellular attachment, bonding, and growth, as shown by the scanning electron microscope (SEM) micrographs in Figure 1[37]. A typical example of the surface roughness of different titanium implants is shown in Table 1. This favorably affects the formation of new tissue and progenitor cells, which are present in almost all tissues[43]. The major role of these progenitor cells is to regulate tissue homeostasis and regeneration upon ageing[20].
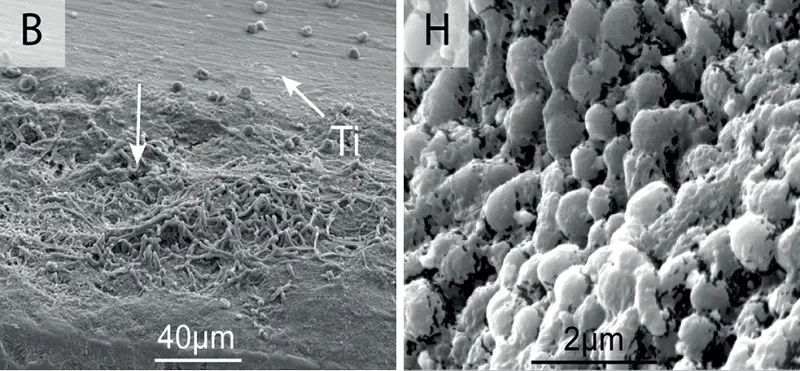
Figure 1. SEM micrographs showing microscopic tissue growth around an implant[37]. SEM: scanning electron microscope.
| Implant | Surface Roughness (μm) | Contact Angle (◦) |
| Biomimetic calcium phosphate (CaP) coating | Ra = 1.83 ± 0.64 | 13.4 ± 0.17 |
| Modified Sandblasted, large grit, acid-etched implant surface (SLA) | Sa = 1.16 ± 0.04 | - |
| Plasma-sprayed hydroxyapatite (HA) coating | Ra = 1.06 ± 0.21 | 57.4 ± 3.2 |
| Commercially pure titanium(cpTi) | Ra = 0.22 ± 0.01 | 55.4 ± 4.1 |
| Titanium Plasma-Sprayed (TPS) | Ra = 7.01 ± 2.09 | - |
| Sandblasted, large grit, acid-etched implant surface (SLA) | Sa = 1.15 ± 0.05 | 138.3 ± 4.2 |
Fundamentally, the functions of stem cells deteriorate with age, possibly through modifications in self-renewal, differentiation potential, senescence, and arrest of proliferation[38]. The reduction of progenitor cells is majorly associated with age-related tissue degeneration as well as reduced potential for regeneration after injury[39].
Researchers in recent times have focused more on the roles of oxidative stress and impaired cellular antioxidant mechanisms in stem cell ageing, which also includes alterations in structures that control the repair of damaged DNA, a decrease in telomere length, and epigenetic changes induced by histone acetylation and methylation[38,32].
These activities are mainly influenced by various cell-intrinsic and cell-extrinsic pathways which impact both stem cells and other minor cells evident in the stem cell niche[42]. Reports have been made and various conclusions confirmed that cell creation, movement, and pluripotency are effectively subdued in stem cells obtained from aged periodontal ligament tissues compared with those from children and adolescents[43]. These numerous research works proposed that aging in adults from young adulthood to late adulthood results in inherent changes in the quantity of regenerative (progenitor) cells which with time restricts the capacity for the development of new tissue formation that in some cases is upturned by delivery of deficient molecular cues to the wound site.
The healing of muscles and bones in the late adulthood stage is usually affected conspicuously by a decelerated capacity to neutralize responsive oxymolecules of the respiratory chain. Free radicals are formed by these respiratory chains and cause oxidative damage to vital cellular constituents which in no time affect cellular function by deteriorating cells of osteogenic lineage[44]. Aging in adults also shows a negative effect on angiogenesis. It can occur at different stages of adulthood including variations in development or signals associated with vascular endothelial growth factor and fibroblast growth factor-2[45].
After implant insertion, the long-term achievement of implant therapy solely depends on the ability of the seal located around soft tissue to be maintained around the implant to yield effective bone support. Effective healing and maturation of wounds and ensuing remodeling are paramount to achieving the entire requirements for clinical success. Thus, comprehending the effects of aging on tissue maturation and remodeling cannot be overemphasized. In aging adults, tissue-remodeling stages in the wound-healing process after dental implantation bring about changes in collagen constituents in the wound. With the maturation of the wound, type III collagen, which is a major matrix compound present in granulation tissue, is ultimately replaced with type I collagen[46]. It has been confirmed that remodeling and maturation of tissues after implantation in aging adults starts with a very high level of proteolytic enzymes which in the long run often show deterioration in the mechanical properties of developing tissue[47]. Aging in adulthood simultaneously enhances apoptotic signaling. It has also been reported that the elimination of cells from newly regenerated tissue is affected by aging[48].
Du et al.[48] in their study reported that in preclinical animal trials, ovariectomized animals exhibit osteoporosis which is detrimental to osseointegration, as revealed by histomorphometry results like the bone-implant contact and bone volume. Thus, applying osteogenic surface modifications on animals is confirmed to enhance osseointegration in comparable preclinical animal models[49]. It has also been revealed in some clinical reports where it was stated that osteoporosis is a risk feature that affects the failure of body implants. However, adequate indications are yet to be made to show that osteoporosis possesses harmful effects on bone healing during or after osseointegration, thus, conclusions cannot be made to prove the relationship between osteoporosis and dental implantation[50].
It is fascinating to know that in most research, implant surgery in adults has been carried out with an average age of 55 years with few post-operative problems confirmed[51]. A regression analysis carried out on 388 Straumann TPS implants confirmed that age is not significantly related to implant survival time[52]. Implantations in senile adults have not been proved lately by researchers to be an issue in terms of slow wound healing or post-operative complications. Nevertheless, senile adults with chronic health challenges should not be administered a dental implant[52].
3. Facial Implants and Age Range
3.1 Facial implants
According to the global statistics carried out by Statista in 2020, facial subdermal implantation is the third most common cosmetic implant administered worldwide[53]. The use of implantable biomaterials has no doubt become an essential part of facial reconstruction as well as aesthetic surgeries due to their efficiency and biodegradability[54]. Facial implants are often used in various applications including post-traumatic reconstruction, correction of congenital abnormalities, and aesthetic augmentation or enhancement[55]. Various augmented facial sites including nasal dorsum, malar eminence, lip, forehead, cheek, and chin in diverse applications (which include orbital floor reconstruction, rhinoplasty, and augmentation of the facial skeleton) have been implemented[56].
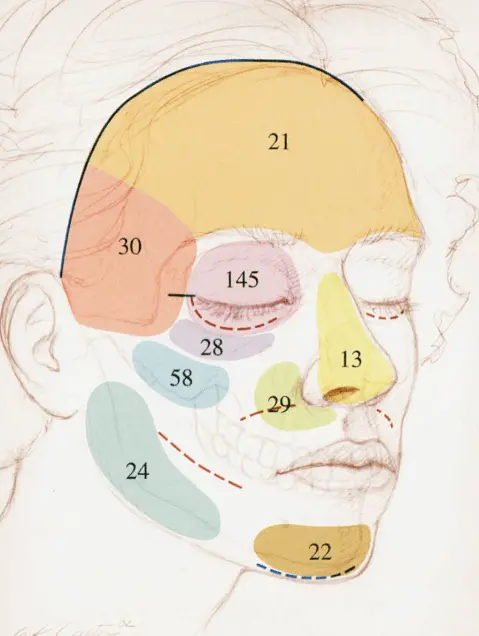
Figure 2 shows the diagram of the application of biomaterials as a facial skeleton and distribution of implants according to anatomical location [Internal Orbit (145); Malar (58); Temporal (30); Paranasal (29); Infraorbital Rim (28); Mandibular Body and Ramus (24); Chin (22); Frontal (21); Nasal (13)]. The blue lines represent cutaneous incisions while the red lines represent mucosal incisions[57].
Autogenous options (bone, cartilage, fat, dermis, fascia, etc.) are often described as the backbone or "gold standard" for introducing changes in the facial profile. Also, the term swapping "self with self" is pertinent to the facial skeleton and soft tissues[58]. Irrespective of their form, biodegradable materials undergo a gradual degradation over a period of time to assist as scaffolds or for the healing process in facial cosmetic or plastic surgery[59]. To perform this task perfectly, the ideal biodegradable implant material used for facial cosmetic or plastic surgery must imitate the characteristics of the tissue to be replaced, augmented, or supported. However, transfer or relocation of autogenous tissue is generally desired at the site of reconstruction or surgical enhancement, graft resorption, and distortion. Also, the unavailability of adequate tissue and donor-site morbidity, in the long run, can be detrimental and as well pose complications to the patient[60].
On the other hand, allogeneic implants have been used for facial plastic surgery for many years as a substitute for autologous grafts, and previous reviews have shown the successful use of several materials to augment contours in the facial skeleton. Hard implants are applied in the restructuring of a variety of maxillofacial defects including frontal and temporal regions, infraorbital rim, paranasal, internal orbit, malar, nasal regions, mandible, and chin. Hard implant materials also offer a more conspicuous substitute to enormous reconstructive sites and exhibit exceptional, natural contours in facial sites that need delicate three-dimensional implantation (for example, nasal dorsal augmentation, and microtia repair).
Commonly used hard implants in facial restructuring include Silicone (polydimethylsiloxane), Gore-Tex (expanded polytetrafluorethylene), MedPor (high-density porous polyethylene), Silastic (solid silicone elastomer) and Mersilene (non-resorbable polyester fiber) while some other ones that are not often used are polymethylmethacrylate (PMMA), Supramid (polyamide nylon mesh) and Permacol (porcine dermal collagen)[61].
In growing pediatric patients, the maxilla is the most traumatized region in the face. After the loss of a tooth that is about 40-60% of bone, resorption occurs in the first year and this happens mainly in the facial plate.
3.2 Children
Granstrom et al.[62] in their study on Osseo-integrated implants in children examined 100 pediatric patients under the age of 16 years who require Osseo-integrated implant surgery. In their research, 76 of these pediatric patients had solid implants administered to them for bone-anchored hearing aids often known as prostheses. In this case, the major indication for the implant installation was a bilateral ear lobe malformation. The implantation was inherently operated as a two-stage process with a healing duration of 3 to 4 months. About 39% of these implants were placed in contact with the dura, sigmoid sinus, or air cell. Granstrom also concluded that a steady follow-up must be followed in pediatric patients after facial implantation because growth is inevitable in pediatric patients which most times affects the position of the implants and in the long run may cause discomfort to the growing patients. Figure 3 is a clear example of the conclusion Granstrom et al.[62] made. An Osseo-integrated implant was inserted in the left ear of an eight-year-old boy. In this case, two Osseo-integrated implants were inserted as a 2-stage procedure, which included abutments and a bar for retention of external ear prosthesis. Constant follow-up gave way to a perfectly implanted Osseo-integrated implant.
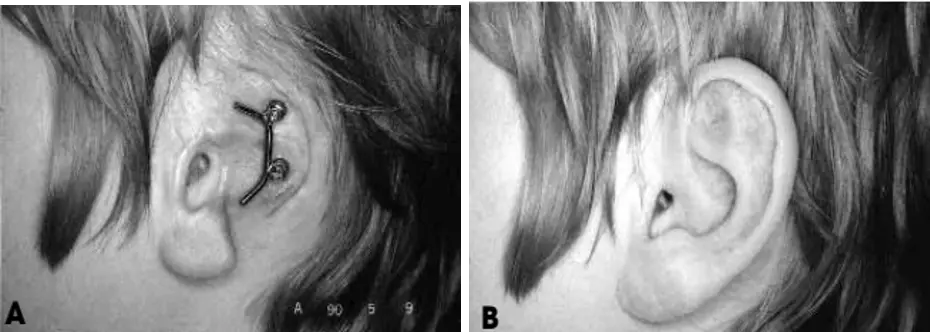
Figure 3. (A) Image of an 8-year-old boy who lost most of his left external ear after a dog bite; (B) prosthesis in place after the lobules are left intact[62].
Granstrom et al.[62] in their study also recorded implant failures in up to 5.8% of 170 inserted fixtures. The presence of adverse skin reactions appeared in 9.1% of the 100 pediatric patients that are less than 16 years old over 21 years post-implant follow-up therapy duration. Modification surgery was embarked on for 22% of patients due to the presence of appositional growth that occurred in the temporal bone. About 24 pediatric patients in the age range of 9-11 years old were not fit for the osseointegration surgery due to their fragile physical state. Cosmetic surgery was measured to be an enhanced alternative to enable the growth of the temporary bone. Granstrom et al.[62] finally reported that the rate of facial implantation failure in children and adolescents is lower when compared to adults because revision surgery is easily carried out in pediatric and early pubertal patients due to the formation of fresh bone, but the occurrence of skin reactions is the same with adults.
3.3 Adolescents and adults
Several research works in previous years have looked at the post-implant results following facial reconstruction in growing and adult patients using different types of facial implant materials. There are also conditional merits and demerits of the varying material type used for facial implantation, with reported complications, irregular contouring of the overlying skin/tissue, infections, extrusion of the implant, mispositioning, pain, or patient discomfort, and in some cases hypoesthesia. Threats and complications faced while administering facial implants is usually grouped based on the material used, the site of the implant, and the maxillofacial movements of the patients after implantation[61].
Infection in the implant site of poorly implanted facial implants has always been an issue of concern, especially in adulthood because these materials possess lower vascular ingrowth and further act as a surface for the colonization of bacteria as well as biofilm formation[63]. As long as facial implantation is concerned, it remains a controversial issue as to whether porous facial implant materials (including MedPor, GoreTex, and Mersilene) possess a high threat of infection when likened to their "fine" counterparts (silicone)[64].
A good number of zealous researchers have taken time to study the infection rates accompanying GoreTex, MedPor, and silicone, and their conclusions are inconsistent due to the differences in age, gender, and environmental factors affecting the implants. Bacterial biofilm formation is also a critical issue to be looked into in orthopedic surgery and ophthalmology implantation and has gained a good number of attention in the field of facial implantation[65]. Biofilms and biofilm formation are significant since they are assumed to affect the confounding events that occur during post-surgery which include prolonged pain, delayed infection, and in worse cases chronic or malignant infection. When compared to orthopedic surgery, the surgical procedures in facial implants are usually clean-contaminated rather than sterile. However, conclusions are yet to be made to confirm the effects of the "clean-contaminated" implant materials on biofilm formation since this formation usually has adverse effects in growing patients[66].
An extensive study made by Berghaus and Stelter[67] reported the high infection risks of adult and aging patients when implanted with porous facial implants by introducing scaffolding for the breeding of bacteria. It is important to know that facial implant materials with smaller pores likely show more risk of infection since they show negativity in the granulation of an extensive tissue and the distribution of host inflammatory cells to improve the immune system of the patients. Complications in adult patients seen with facial implantation usually occur due to inadequate correction or over-correction, infection, extrusion, malposition, implant migration, nerve hypesthesia/anesthesia, and facial nerve injury[68].
A prominent position on the face is the nose which is amenable to micro-trauma and major blows and increases infection risk as well. Pre-operative or intra-operative shaping of implants is not just an important but also a delicate step in the prevention of complications in any age range of human growth[56]. Complications also occur in patients with somatic diseases which makes the usage of implants challenging and sometimes impossible. Several cases of somatic delusions and delusional halitosis have been observed and researched by several authors[69]. Some patients suffering from body dysmorphic disorders also most times oppose implantation[70]. These patients have to undergo treatment for these psychiatric issues before they can undergo any type of facial implantation[71].
4. Future Demand
From the reviewed research reports, it was obvious that more efforts are to be focused on the development of advanced implant materials for the various and complex body parts that demand flexibility. Presently, the use of smart materials in some respects is not capable of solving some maxillofacial prosthesis and dental implantation challenges. The influence of growth or the consideration of age group and the risk factors for each age group, in the development of suitable implants is still an issue to be well thought out while considering materials for this application[15]. Therefore, there is a need to look into how to advance seemly materials in the future. Nanotechnology is currently one of the methods for achieving advanced and dynamic materials. Hence, the application of nanomaterials as well as smart materials can be considered in meeting the ever-evolving and dynamic requirements in this field. This is pertinent because adopting only nanotechnology for the production of these advanced materials may not satisfy the ever-increasing properties desirable for satisfactory performance[11]. It is expected that researchers will still create more advanced processing routes for the development of novel materials that can meet any expected needs[8]. Future demands for advanced cosmetics and fashion materials need to be expected, hence, the need for more flexible technologically oriented materials and process development. A proper guide will be needed for classifications of biomedical implants with respect to age groups as; childhood implants, adolescent implants, and adult implants that focus on challenges that are common to each group. With this, it will be easier to group materials, search for materials, and process these materials for desired properties and applications in biomedical industries.
5. Conclusion
This review has revealed that age and growth are fundamental to the development of maxillofacial prosthesis and dental implant devices which are very useful in the management of a wide variety of maxillofacial and dental ailments. The selection of suitable materials depends on certain factors, including the age of the individual which determines the level of biological activities going on within the age range and growth rate, materials used in manufacturing implants or prosthetics, and the nature of the ailment. There is an inevitable change in the effectiveness of implants in humans as they grow older from infants through adolescents to adults. The reason for this is that infants will require constant implant replacements as they grow older into adolescents, while adults do not require as much change upon implant fixation. The nature of the ailments has also proven to have a profound effect on the type of implants used and the duration of implantation. These factors have directly affected the need for maintenance of the implants and prosthetics, as well as their manufacturing requirements to avoid post-surgical complications. It was discovered from the review that, the attention needed by the children and adolescents are similar because they are still growing while for adults, adequate healing is the major concern as it may take a longer time for healing to take place due to less active biological activities at older age. Therefore, a direct correlation can be drawn between the age of the individual, the materials used for the manufacturing of implants, the rate or efficiency of the healing process, and the type of post-implantation culture to be adopted.
Acknowledgements
The authors wish to acknowledge the assistance of the management of Federal University of Technology Akure Nigeria for providing the facilities needed for the collation of materials.
Author contributions
Oladele IO: Conceptualization of the idea and correction.
Onuh LN: Collation of materials and writing.
Taiwo AS: Correction and editing.
Agbeboh NI: Writing of the paper.
Adegun MH: Provision of materials.
Conflicts of interest
The authors declare no conflict of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
None.
Copyright
© The Author(s) 2023.
References
-
1. Zimmerman B, Shumway KR, Jenzer AC. Physiology, Tooth. Treasure Island: StatPearls; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538475/
-
2. Yan R, Chen X, Gong X, Wang J, Yu J. The association of tooth loss, toothbrushing, and quality of life among cancer survivors. Cancer Med. 2018;7(12):6374-6384.[DOI]
-
3. Griggs JA. Dental implants. Dent Clin North Am. 2017;61(4):857-871.[DOI]
-
4. De Souza N, Manju R, Hegde AM. Development and evaluation of new clinical methods of age estimation in children based on the eruption status of primary teeth. J Indian Soc Pedod Prev Dent. 2018;36(2):185-190.[DOI]
-
5. Annibali S, Cristalli MP, Dell'Aquila D, Bignozzi I, La Monaca G, Pilloni A. Short dental implants: a systematic review. J Dent Res. 2012;91(1):25-32.[DOI]
-
6. Watt RG. Teeth and inequality: from past to present. Lancet. 2018;391(10138):2406.[DOI]
-
7. Oladele IO, Taiwo AS, Onuh LN, Adelani SO, Balogun SO, Lephuthing SS, et al. Characterization of animal shells-derived hydroxyapatite reinforced epoxy bio-composites. Compos Adv Mater. 2023;32:1-13.[DOI]
-
8. Oladele IO, Omotosho TF, Ogunwande GS, Owa FA. A review on the philosophies for the advancement of polymer-based composites: Past, present and future perspective. Appl Sci Eng. 2021;14(4):553-579.[DOI]
-
9. Agbabiaka OG, Oladele IO, Akinwekomi AD, Adediran AA, Balogun AO, Olasunkanm OG, et al. Effect of calcination temperature on hydroxyapatite developed from waste poultry eggshell. Sci Afr. 2020;8:e00452.[DOI]
-
10. Kamatham R, Avisa P, Vinnakota DN, Nuvvula S. Adverse effects of implants in children and adolescents: A systematic review. J Clin Pediatr Dent. 2019;43(2):69-77.[DOI]
-
11. Oladele IO, Omotosho TF, Adediran AA. Polymer-based composites: an indispensable material for present and future applications. Int J Polym Sci. 2020;2020(1):8834518.[DOI]
-
12. Muhamad AH, Azzaldeen A, Maria A, Chlorokostas G. Dental Implants in Children: An Update. J Oral Health Dent Res. 2021;2(1):1-9. Available from: https://manuscriptscientific.com/51dd72.pdf
-
13. Brahim JS. Dental implants in children. Oral Maxillofac Surg Clin North Am. 2005;17(4):375-381.[DOI]
-
14. Muhamad AH, Azzaldeen A, Nezar W, Mohammed Z. Congenitally missing lateral incisor with orthodontics, bone grafting and single-tooth implant: a case report. J Dent Med Sci. 2015;14(4):124-130.[DOI]
-
15. Oladele IO, Onuh LN, Agbeboh NI, Alewi DD, Lephuthing SS. The relationship and functional links between human age, growth, and biomedical implants: A review on the application of bulk and nanomaterials. Nano Sel. 2023;4(7):419-441.[DOI]
-
16. Srinivasan M, Meyer S, Mombelli A, Müller F. Dental implants in the elderly population: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28(8):920-930.[DOI]
-
17. Arhakis A, Boutiou E. Etiology, diagnosis, consequences and treatment of infraoccluded primary molars. Open Dent J. 2016;10:714-726.[DOI]
-
18. Sheng L, Silvestrin T, Zhan J, Wu L, Zhao Q, Cao Z, et al. Replacement of severely traumatized teeth with immediate implants and immediate loading: literature review and case reports. Dent Traumatol. 2015;31(6):493-503.[DOI]
-
19. Sharma P, Arora A, Valiathan A. Age changes of jaws and soft tissue profile. Sci World J. 2014;2014:201501.[DOI]
-
20. Gobbato L, Paniz G, Mazzocco F, Wang CW. Multidisciplinary management of a young female with infraoccluded dental implants: a case report. Int J Esthet Dent. 2016;11(2):162-173.[PubMed]
-
21. Giannetti L, Murri Dello Diago A, Vecci F, Consolo U. Mini-implants in growing patients: A case report. Pediatr Dent. 2010;32(3):239-244.[PubMed]
-
22. Kumari S, Nichani MH, Hariharan VS. Dental implants in children and adolescents. Indian J Multidiscip Dent. 2010;1(1):50-54.
-
23. Sharma AB, Vargervik K. Using implants for the growing child. J Calif Dent Assoc. 2006;34(9):719-724.[DOI]
-
24. Fernandes APS, Battistella MA. Dental Implants in Pediatric Dentistry: A Literature Review. Braz J Implantol Health Sci. 2020;2(2):1-12.
-
25. Walter C, Al-Nawas B, Wolff T, Schiegnitz E, Grotz KA. Dental implants in patients treated with antiresorptive medication - a systematic literature review. Int J Implant Dent. 2016;2(1):9.[DOI]
-
26. Thilander B, Odman J, Lekholm U. Orthodontic aspects of the use of oral implants in adolescents: a 10-year follow-up study. Eur J Orthod. 2001;23(6):715-731.[DOI]
-
27. Bohner L, Hanisch M, Kleinheinz J, Jung S. Dental implants in growing patients: a systematic review. Br J Oral Maxillofac Surg. 2019;57(5):397-406.[DOI]
-
28. Jivraj S, Chee W. Treatment planning of implants in the aesthetic zone. Br Dent J. 2006;201(2):77-89.[DOI]
-
29. Schneider D, Witt L, Hammerle CHF. Influence of the crown-to-implant length ratio on the clinical performance of implants supporting single crown restorations: a cross-sectional retrospective 5-year investigation. Clin Oral Implants Res. 2012;23(2):169-174.[DOI]
-
30. Schulte J, Flores AM, Weed M. Crown-to-implant ratios of single tooth implant-supported restorations. J Prosthet Dent. 2007;98(1):1-5.[DOI]
-
31. Ledermann PD, Hassell TM, Hefti AF. Osseointegrated dental implants as alternative therapy to bridge construction or orthodontics in young patients: seven years of clinical experience. Pediatr Dent. 1993;15(5):327-333.[PubMed]
-
32. Bartold PM, Ivanovski S, Darby I. Implants for the aged patient: biological, clinical and sociological considerations. Periodontology 2000. 2016;72(1):120-134.[DOI]
-
33. Donos N, Hamlet S, Lang NP, Salvi GE, Huynh-Ba G, Bosshardt DD, et al. Gene expression profile of osseointegration of a hydrophilic compared with a hydrophobic microrough implant surface. Clin Oral Implants Res. 2011;22(4):365-372.[DOI]
-
34. Ivanovski S, Hamlet S, Retzepi M, Wall I, Donos N. Transcriptional profiling of "guided bone regeneration" in a critical-size calvarial defect. Clin Oral Implants Res. 2011;22(4):382-389.[DOI]
-
35. Doles J, Storer M, Cozzuto L, Roma G, Keyes WM. Age-associated inflammation inhibits epidermal stem cell function. Genes Dev. 2012;26(19):2144-2153.[DOI]
-
36. Gomez MG, Aguilar SA, Rubio RJ, Guardia J, Gargallo J, Calvo-Guirado JL. Peri-implant evaluation in type 2 diabetes mellitus patients: a 3-year study. Clin Oral Implants Res. 2015;26(9):1031-1035.[DOI]
-
37. Anitua E, Alkhraisat MH, Tejero R. Immediate replacement of failed dental implants owing to periimplantitis. J Oral Rehabil. 2015;1:8-14. Available from: https://www.implante.institute/artigo
-
38. Hadjiargyrou M, O'Keefe RJ. The convergence of fracture repair and stem cells: interplay of genes, aging, environmental factors and disease. J Bone Miner Res. 2014;29(11):2307-2322.[DOI]
-
39. Richardson GD, Breault D, Horrocks G, Cormack S, Hole N, Owens WA. Telomerase expression in the mammalian heart. FASEB J. 2012;26(12):4832-4840.[DOI]
-
40. Jung Y, Brack AS. Cellular mechanisms of somatic stem cell aging. Curr Top Dev Biol. 2014;107:405-438.[DOI]
-
41. Bagno A, Di Bello C. Surface treatments and roughness properties of Ti-based biomaterials. J Mater Sci Mater Med. 2004;15(9):935-949.[DOI]
-
42. Le Guehennec, Soueidan A, Layrolle P, Amouriq Y. Surface treatments of titanium dental implants for rapid osseointegration. Dent Mater. 2007;23(7):844-854.[DOI]
-
43. Zhang J, An Y, Gao LN, Zhang YJ, Jin Y, Chen FM. The effect of aging on the pluripotential capacity and regenerative potential of human periodontal ligament stem cells. Biomaterials. 2012;33(29):6974-6986.[DOI]
-
44. Kloss FR, Gassner R. Bone and aging: effects on the maxillofacial skeleton. Exp Gerontol. 2006;41(2):123-129.[DOI]
-
45. Gunin AG, Petrov VV, Golubtzova NN, Vasilieva OV, Kornilova NK. Age-related changes in angiogenesis in human dermis. Exp Gerontol. 2014;55(1):143-151.[DOI]
-
46. Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature. 2008;453(7193):314-321.[DOI]
-
47. Smith PC, Caceres M, Martinez C, Oyarzun A, Martinez J. Gingival wound healing: an essential response disturbed by aging? J Dent Res. 2015;94(3):395-402.[DOI]
-
48. Du Z, Chen J, Yan F, Doan N, Ivanovski S, Xiao Y. Serum bone formation marker correlation with improved osseointegration in osteoporotic rats treated with simvastatin. Clin Oral Implants Res. 2013;24(4):422-427.[DOI]
-
49. Javed F, Vohra F, Zafar S, Almas K. Significance of osteogenic surface coatings on implants to enhance osseointegration under osteoporotic-like conditions. Implant Dent. 2014;23(6):679-686.[DOI]
-
50. Giro G, Chambrone L, Goldstein A, Rodrigues JA, Zenobio E, Feres M, et al. Impact of osteoporosis in dental implants: a systematic review. World J Orthop. 2015;6(2):311-315.[DOI]
-
51. van Velzen FJJ, Ofec R, Schulten EAJM, ten Bruggenkate CM. 10-year survival rate and the incidence of peri - implant disease of 374 titanium dental implants with a SLA surface: a prospective cohort study in 177 fully and partially edentulous patients. Clin Oral Implants Res. 2015;26(10):1121-1128.[DOI]
-
52. Lee HJ, Kim YK, Park JY, Kim SG, Kim MJ, Yun PY. Short-term clinical retrospective study of implants in geriatric patients older than 70 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(4):442-446.[DOI]
-
53. Michas F. Top Surgical Costmetic Procedures Worldwide in 2020 [Internet]. 2022.
-
54. Rojas YA, Sinnott C, Colasante C, Samas J, Reish RG. Facial implants: controversies and criticism. A comprehensive review of the current literature. Plast Reconst Surg. 2018;142(4):991-999.[DOI]
-
55. Oliver JD, Eells AC, Saba ES, Boczar D, Restrepo DJ, Huayllani MT, et al. Alloplastic facial implants: a systematic review and meta-analysis on outcomes and uses in aesthetic and reconstructive plastic surgery. Aesthetic Plast Surg. 2019;43(3):625-636.[DOI]
-
56. Cuzalina LA, Hlavacek MR. Complications of facial implants. Oral Maxillofac Surg Clin North Am. 2009;21(1):91-104.[DOI]
-
57. Yaremchuk MJ. Facial skeletal reconstruction using porous polyethylene implants. Plast Reconst Surg. 2003;111(6):1818-1827.[DOI]
-
58. Goldsmith D, Horowitz A, Orentlicher G. Facial skeletal augmentation using custom facial implants. Atlas Oral Maxillofac Surg Clin North Am. 2012;20(1):119-134.[DOI]
-
59. Prakasam M, Locs J, Salma-Ancane K, Loca D, Largeteau A, Berzina-Cimdina L. Biodegradable materials and metallic implants - a review. J Funct Biomater. 2017;8(4):44.[DOI]
-
60. Quatela VC, Chow J. Synthetic facial implants. Facial Plast Surg Clin North Am. 2008;16(1):1-10.[DOI]
-
61. Patel K, Brandstetter K. Solid implants in facial plastic surgery: potential complications and how to prevent them. Facial Plast Surg. 2016;32(5):520-531.[DOI]
-
62. Granstrom G, Bergstrom K, Odersjo M, Tjellstrom A. Osseointegrated implants in children: experience from our first 100 patients. Otolaryngol Head Neck Surg. 2001;125(1):85-92.[DOI]
-
63. Walker TJ, Toriumi DM. Analysis of facial implants for bacterial biofilm formation using scanning electron microscopy. JAMA Facial Plast Surg. 2016;18(4):299-304.[DOI]
-
64. Ridwan-Pramana A, Wolff J, Raziei A, Ashton-James CE, Forouzanfar T. Porous polyethylene implants in facial reconstruction: Outcome and complications. J Maxillofac Surg. 2015;43(8):1330-1334.[DOI]
-
65. Desai SC, Moradzadeh A, Branham G. Anatomical evidence of microbial biofilms in an alloplastic nasal implant. Aesthetic Plast Surg. 2013;37(2):468-471.[DOI]
-
66. Romo T, Pearson JM. Nasal implants. Facial Plast Surg Clin North Am. 2008;16(1):123-132.[DOI]
-
67. Berghaus A, Stelter K. Alloplastic materials in rhinoplasty. Curr Opin Otolaryngol Head Neck Surg. 2006;14(4):270-277.[DOI]
-
68. Brandt MG, Moore CC. Implants in facial skeletal augmentation. Curr Opin Otolaryngol Head Neck Surg. 2013;21(4):396-399.[DOI]
-
69. Niazi TM, Ulaganathan G, Kalaiselvan S, Lambodharan R, Mahalakshmi R, Sophia M, et al. Dental Implants: A Remote Option in Case of Somatic Delusion Disorder. J Pharm Bioallied Sci. 2017;9(Suppl 1):S257-S260.[DOI]
-
70. Akpata O, Omoregie OF, Akhigbe K, Ehikhamenor EE. Evaluation of oral and extra-oral factors predisposing to delusional halitosis. Ghana Med J. 2009;43(2):61-64.[DOI]
-
71. Uguru C, Umeanuka O, Uguru NP, Adigun O, Edafioghor O. The delusion of halitosis: Experience at an eastern Nigerian tertiary hospital. Niger J Med. 2011;20(2):236-240. Available from: https://www.researchgate.net/publication/51692779_The_delusion_of_halitosis_experience_at_an_eastern_Nigerian_tertiary_hospital
Copyright
© The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Publisher’s Note
Share And Cite